 In the 1939 Technicolor movie marvel The Wizard of Oz, Dorothy asks, as she, the Scarecrow, the Tin Man, and the Cowardly Lion are being made over in the Emerald City, “Can you dye my eyes to match my gown?” Two helpers nod in the affirmative. Until recent decades, the idea that you could change your eye color seemed about as probable as a house falling onto a witch and killing her. But with opaque color contact lenses, even people with the darkest eyes can change eye color to something traditional, like blue, green, or hazel, or to something exotic, like violet, silvery-gray, or honey colored.
In the 1939 Technicolor movie marvel The Wizard of Oz, Dorothy asks, as she, the Scarecrow, the Tin Man, and the Cowardly Lion are being made over in the Emerald City, “Can you dye my eyes to match my gown?” Two helpers nod in the affirmative. Until recent decades, the idea that you could change your eye color seemed about as probable as a house falling onto a witch and killing her. But with opaque color contact lenses, even people with the darkest eyes can change eye color to something traditional, like blue, green, or hazel, or to something exotic, like violet, silvery-gray, or honey colored.
Not only have color contact lenses become mainstream and a popular way for people to change their look, but you can also now easily order contact lenses by post. In the U.S. a valid prescription from an eye doctor is required, even for “Plano” lenses, which are colored contact lenses that do not correct vision and are for effect only. While such exotic lenses used to be only for theatrical use, they are now available to the masses at prices that many people can afford. Color contact lenses can be purchased from many online sellers that also offer eyeglasses.
Types of color contact lenses
The types of color contact lenses available fall into three categories: visibility tint (only enough tint to make contact lenses easier to see when inserting and cleaning), enhancement tint (which subtly alter the color of light-colored eyes), and opaque color tint (which can change any color eye to any other color).
Colored contact lenses are more expensive than plain clear contact lenses. The extra cost is due to the added research done by the companies who make them. The tinting process itself is an added production expense, and because they are produced in smaller quantities than traditional clear contact lenses, they do not achieve the same economies of scale. But because they are becoming more popular all the time, this last reason is becoming less of a factor.
Change your eye color
One of the most dramatic ways of changing your look is by changing your eye color. While older opaque color contact lenses tended to look frankly fake, the newer ones blend several colors into the main color to give them a more natural appearance. The center of the lens is still kept clear for visibility and only the part that covers the iris (the colored part of the eye) is colored.
An annoyance with earlier opaque contact lenses was that they moved enough when the wearer blinked that the contacts shifted and temporarily placed the colored part of the lens partially over the pupil, affecting vision for a split second after blinking. The clear “pupil” of color contact lenses is of a fixed size, though the pupil of the eye changes size according to light conditions. The problem was more pronounced in low light situations because the enlarged pupil was more likely to be partially obstructed by the colored part of the lens. Newer versions of color contact lenses, however, are designed to stay in place better and minimize this problem.
 Ciba Vision
Ciba Vision
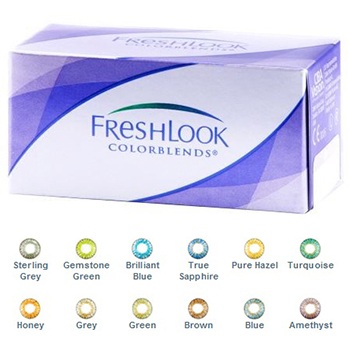
You can order contact lenses by post from several brands. One of the biggest brands is Ciba Vision, maker of FreshLook, FreshLook One-Day, FreshLook Dimensions, and Freshlook Colorblends. FreshLook is one of the most popular selling lines of colored contact lenses today, with colors both subtle and bold. People who do not need vision correction can order FreshLook colored contacts with no vision correction built in. In other words, they change eye color without changing the wearer’s vision.
FreshLook colored contacts are made to be very comfortable. They come in extended wear versions, daily disposables, and one-week disposables. They can also be worn as daily wear lenses (removed and stored overnight) for up to two weeks before they should be discarded. Fresh Look lenses come in boxes of six lenses each. For daily wear, one box would last for six weeks.
FreshLook color contact lenses contain a large clear area over the pupil so that any shifting of the opaque part of the lens is much less likely to affect vision by sliding over the eye’s pupil when the wearer blinks.
FreshLook Dimensions contacts are designed to add enhanced color to naturally light colored eyes, and they are available in Pacific Blue, Caribbean Aqua, and Sea Green. FreshLook Colors and FreshLook Colorblends are opaque colored contacts that can change even dark eyes to any other color.
Acuvue
Acuvue is another brand of color contact lenses. Acuvue is easily one of the top brands of contact lenses and has a reputation for high quality and comfort. Acuvue is owned by the parent company of Johnson & Johnson and is sold all over the world. Acuvue Oasys contact lenses are made with Hydraclear, a material designed to keep eyes moist and comfortable. They can be worn up to one week continuously. They also have high oxygen permeability and are impregnated with moisture-rich wetting agents. They can be made to correct for nearsightedness, farsightedness, and astigmatism and also protect against approximately 96% of UVA and 99% of UVB rays.
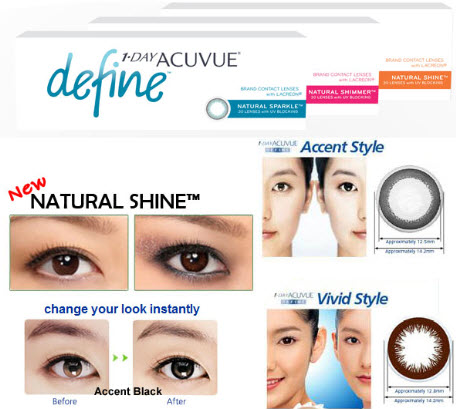 One Day Acuvue disposable lenses are designed to be worn for one day only and then thrown away. It is hard to beat the comfort of a brand-new pair of contacts every day. Because they are dailies, users don’t have to use storage or cleaning solutions. One Day Acuvue lenses are very convenient for traveling, block UV light and are very comfortable for allergy sufferers, whereas traditional contact lenses are worn for several days or weeks risk build-up of pollen, dust, and other allergens.
One Day Acuvue disposable lenses are designed to be worn for one day only and then thrown away. It is hard to beat the comfort of a brand-new pair of contacts every day. Because they are dailies, users don’t have to use storage or cleaning solutions. One Day Acuvue lenses are very convenient for traveling, block UV light and are very comfortable for allergy sufferers, whereas traditional contact lenses are worn for several days or weeks risk build-up of pollen, dust, and other allergens.
Focus is another brand made by contact lens giant Ciba Vision. Focus Dailies are one of the best-selling brands of daily disposable contact lenses. Other Focus disposable contact lenses include Focus Dailies AquaComfort, Focus 1-2 Week, Focus Dailies Toric, Focus and SoftColors.
Most of the color contact lenses sold online are made by Ciba Vision and their many contact lens brands. Ordering contact lenses by post is very easy and only requires an internet connection, a prescription, and a credit card. Millions of people worldwide enjoy the convenience of ordering colored lenses through the internet. Prices are often significantly lower than the prices at opticians’ offices, who frequently have to order your prescription anyway if they don’t happen to have your brand and prescription in stock.
Though regular eye care is important for detecting changes in vision, between eye care appointments (which are usually recommended yearly), ordering contact lenses by post is the best solution for most contact lens wearers. It is also a fun way to order inexpensive color contact lenses, which are an easy way of changing your look. Whether you want to have the same eye color every day, or a selection of colors to choose from, there are dozens of reputable online sellers of contact lenses, with very reasonable prices and quick shipping.
And because contact lenses are so small and lightweight, shipping charges do not have to be very high. It is important, however, to compare shipping charges when comparison shopping for color contact lenses, because sometimes very low-priced lenses come with high shipping costs, which can make them less of a bargain.
Special effects contact lenses
In addition to colored contacts, many online contact lens dealers also sell special effect lenses. These lenses are made with unusual colors and patterns, and are perhaps most popular around Halloween, because of the range of strange effects available. Lenses with spirals, starburst patterns, cat-eye pupils, and even teeth design, so that an eye looks like a mouth full of jagged, pointy teeth!
These too require a doctor’s prescription because even though they do not correct vision, they are contact lenses, and in the U.S. fall under the purview of the Food and Drug Administration. Beware of businesses that sell special effects contact lenses and do not ask for a prescription, because often their suppliers do not have the level of quality control that known brands and known sellers do.
Anyone buying contact lenses must be diligent about safe handling, insertion, removal, and cleaning. Contact lenses should never be shared because of the high risk of eye infection. You must always handle them with clean hands and store them in the recommended solution in a clean contact lens case. That said, contact lenses for vision correction (with or without color) are superior to eyeglasses in many ways. They do not break, they provide optimum vision correction, and peripheral vision from contact lenses is far better than with eyeglasses. Today’s lenses are made from high-tech materials designed to keep eyes moist and comfortable.
Today’s color contact lenses represent a vast improvement over the first-generation colored contacts, which often looked unnatural and caused problems from sliding up or down over the pupil during blinking, temporarily partially blocking vision before sliding back into place on the eye. The colors today often consist of blends of different colors in addition to the main color, more closely mimicking the natural coloration of irises, which do not have uniform coloration, but several shades blended in intricate patterns. And the number of colors available has exploded. Even someone with the darkest brown eyes can have eyes of sapphire blue, amethyst, honey, or pale green.
The world of color contact lenses also includes fun special effects lenses, which almost always come without vision correction. People buy these contact lenses by post because of the convenience and good prices. Although buying colored contacts over the internet is the ultimate in comfort and often savings, anyone who wears contact lenses – even solely as fashion accessories – should maintain regular eye care appointments so that any changes in prescription can be noted, and so an eye care professional can recommend the best brands for a person’s particular eye anatomy and needs.